As you get ready to attend the United States Conference on AIDS (http://www.2012USCA.org), here is a potential new model for HIV prevention and care services to be discussed at this year’s meeting. Hopefully, this will be one of many models to review. This model incorporates the recent bio-medical advancements [e.g. Treatment as Prevention (TasP), Pre-Exposure Prophylaxis (PrEP), etc.] with the implementation of the National HIV/AIDS Strategy (NHAS) for the U.S. and the Affordable Care Act (ACA).
 The National Minority AIDS Council’s (NMAC) model for HIV prevention and care is based on modeling done by Dr. David Holtgrave and published in May of this year. The premise of this model is to move people living with HIV/AIDS (PLWHA) along the treatment cascade so that approximately 81% of people living with HIV in the U.S. know their HIV status and have a suppressed viral load. This is both ambitious and necessary to end the HIV epidemic here at home. This model asks Health Departments (HDs) and Community Based Organizations (CBOs) to:
The National Minority AIDS Council’s (NMAC) model for HIV prevention and care is based on modeling done by Dr. David Holtgrave and published in May of this year. The premise of this model is to move people living with HIV/AIDS (PLWHA) along the treatment cascade so that approximately 81% of people living with HIV in the U.S. know their HIV status and have a suppressed viral load. This is both ambitious and necessary to end the HIV epidemic here at home. This model asks Health Departments (HDs) and Community Based Organizations (CBOs) to:
- Identify people who do not know they are HIV positive
- Increase linkage to and retention of PLWHA in high-quality care, and
- Improve treatment adherence among PLWHA to achieve a suppressed viral load
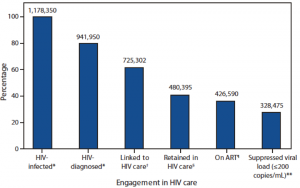
Current Treatment Cascade
__________________________________________________________________
Ideal Treatment Cascade
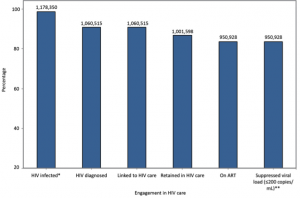 As you will notice from the above two graphs, the premise of this model is to move PLWHA along the cascade so that there is very little drop off between the number of those who know they’re HIV-positive and those who are engaged in care and achieve an undetectable viral load. Using this model, HDs and CBOs will be able to measure change, identify successes, and end the HIV/AIDS epidemic in America. One important caveat here is that Dr. Holtgrave’s model is based on a significant increase in prevention and care dollars. While increases on this scale over the next couple of years are unlikely, we should still work to ensure the best possible outcomes with the resources we have available, while continuing to press for the resources needed to get the job done.
As you will notice from the above two graphs, the premise of this model is to move PLWHA along the cascade so that there is very little drop off between the number of those who know they’re HIV-positive and those who are engaged in care and achieve an undetectable viral load. Using this model, HDs and CBOs will be able to measure change, identify successes, and end the HIV/AIDS epidemic in America. One important caveat here is that Dr. Holtgrave’s model is based on a significant increase in prevention and care dollars. While increases on this scale over the next couple of years are unlikely, we should still work to ensure the best possible outcomes with the resources we have available, while continuing to press for the resources needed to get the job done.
Each phase of this model requires a specific set of testing, retention and care services. Health Departments will play a critical role in coordinating service provision and access. The success of this model will be determined by the degree to which services providers are able to improve and sustain health outcomes in each area measured in the cascade. NMAC recommends a focus on
- HIV testing (with a focus on tapping into networks to identify unknown positives)
- Linkage to and Retention in high quality care
- Education and support to help PLWHA incorporate into their lives in a sustainable fashion
Goal – HIV Testing
 The CDC’s Vital Signs report on HIV prevention through treatment and care estimates that we have 1.2 million living in the United States who are HIV positive. Around 942,000 PLWHA are aware of their sero-positivity, with around 258,000 unaware. HIV testing technology and counseling services for HIV-negative and HIV-positive persons must be included in each state’s essential health benefits package under the ACA, with additional funds for testing used to diagnose those who may still not be engaged in the health care system, especially highly impacted and marginalized populations. Given the limited HIV prevention funds, testing initiatives should be strategic and focus on reaching gay men, transgender individuals, African American women and Latinas.
The CDC’s Vital Signs report on HIV prevention through treatment and care estimates that we have 1.2 million living in the United States who are HIV positive. Around 942,000 PLWHA are aware of their sero-positivity, with around 258,000 unaware. HIV testing technology and counseling services for HIV-negative and HIV-positive persons must be included in each state’s essential health benefits package under the ACA, with additional funds for testing used to diagnose those who may still not be engaged in the health care system, especially highly impacted and marginalized populations. Given the limited HIV prevention funds, testing initiatives should be strategic and focus on reaching gay men, transgender individuals, African American women and Latinas.
Linkage and Retention To Care
Vital Signs says that around 725,300 PLWHA are linked to care and around 480,400 are retained in care. This is where the ACA will hopefully make a significant difference in our ability to care for PLWHA. Our goals should be for all PLWHA to be retained in care. HIV is a disease that needs to be monitored by health care professionals. ACA gives us a pathway to make that a reality.
We are talking about moving an additional 461,600 PLWHA onto private insurance and/or Medicaid/Medicare. Existing healthcare systems do not have the capacity to identify and retain all these new clients. This is where the HIV community has learned many lessons and can provide critical support to ensure people do not fall out of care or fall through the cracks.
Our history tells us that it’s not enough just to see a health care professional. Our continuum of care model has shown us that successful care is patient focused and provides linkages to other vital services such as housing. Our recommendation is thatvoluntary prevention case management be available to all people living with HIV/AIDS. This program will link health care to HIV prevention. It will work with and support HIV-positive individuals by connecting them to the appropriate health care system, monitoring their progress, providing case management for non-medical services while working to prevent new HIV infections via prevention for positives. Ultimately all PLWHA should have access to this form of voluntary case management.
It is also critical to develop programming that addresses stigma, which continues to be a major barrier to retention and adherence. This includes efforts to repeal HIV criminalization statues, which can discourage testing and disclosure.
HIV Treatment/ Viral Load Suppression and Sustainability
 HIV treatment should be available to all PLWHA. Once again, this is where the ACA will make a significant difference. According to Vital Signs, among HIV-infected adults in care, 89% were prescribed antiretroviral therapy (ART), of whom 77% had viral suppression. Although this number sounds high, in reality, only 28% or 328,475 of all PLWHA had a suppressed viral load.
HIV treatment should be available to all PLWHA. Once again, this is where the ACA will make a significant difference. According to Vital Signs, among HIV-infected adults in care, 89% were prescribed antiretroviral therapy (ART), of whom 77% had viral suppression. Although this number sounds high, in reality, only 28% or 328,475 of all PLWHA had a suppressed viral load.
Given the challenges of HIV adherence, nobody should be forced to take HIV medications. It must be a choice. That is why NMAC recommends comprehensive treatment education and adherence services be made available to all PLWHA. HDs should work with CBOs to insure quality treatment education programs and specialized treatment navigators are available to support PLWHA efforts.
To achieve the goals of this model, we need an additional 622,400 PLWHA to be able to sustain an undetectable viral load over an extended period of time. That will not happen without support and education. NMAC believes that treatment navigators are the best and most cost efficient way to achieve this goal.
Additionally, any new system of programs, interventions, and/or capacity building activities should align with the goals of this model. Given the fact that we will still be operating with limited resources, interventions should be cost effective, target highly impacted populations, and used in combination with other interventions, prioritizing the programs that will reduce the largest number of HIV infections.
We have lots to discuss at this year’s USCA. Decisions we make today will impact our movement for the next decade. This is just one proposed model. That is why we need you to come to this year’s meeting prepared to discuss, debate and analyze options on how we can end the HIV/AIDS epidemic in America. I look forward to seeing you in Las Vegas.
Yours in the struggle,
Paul Kawata
Executive Director
National Minority AIDS Council